In 1966 the television series “Star Trek” brought a fictional universe with faster-than-light space travel and aliens called Vulcans to the living rooms of America. And an old country doctor named Leonard “Bones” McCoy used a handheld device to diagnose and collect bodily information about a patient in a matter of seconds.
A year later the science fiction film “2001: A Space Odyssey” debuted in movie theaters and has since been recognized by many critics and audiences as one of the greatest films ever made. What made the movie so distinct were the thematic elements of human evolution, technology and, certainly, the introduction of artificial intelligence that went by the name of HAL.
Then in the mid-1970s, two top-grossing films brought science fiction back to mainstream. While “Close Encounters of the Third Kind” and “Star Wars” captured the country’s imagination, William Hauswirth and his colleagues at the University of Florida imagined helping blind people see.
The UF College of Medicine doesn’t exactly have the look or feel of a science fiction movie set or the make-believe bridge of the starship Enterprise. But a closer look into some of the science and treatment methods being researched, taught and tested here reveal a strong resemblance to a few of our favorite sci-fi special effects. In 2001 a multi-university team that included Hauswirth and fellow geneticists restored sight in blind puppies born with a genetic defect by inserting a corrective gene into their eyes. Now that gene-transfer technique is being tested on humans in a phase 1 clinical study. Preliminary results indicate the gene therapy is not only safe for patients, but effective in restoring vision.
UF emergency medicine faculty are testing a wireless device the size of a cell phone that measures, stores and transmits a variety of patient vital signs from a distance. Similar to Dr. McCoy’s tricorder, the real-world device has the potential to help medical responders immediately determine which patients need care first. But the closest example to science fiction at UF may be the recent discovery from a team of medical and engineering researchers who are developing devices that allow a person to control a robotic limb with just their thoughts. The group reported in September it has discovered a way for the brain-machine interface to actually evolve with the brain as it learns.
We can rebuild them.
We have the technology.
MEDICAL SHIP, Somewhere in Space – With his arm stretched in front of him, Luke Skywalker watches as the robot fiddles with the wiring of his new prosthetic hand. A silver contraption with needle-thin wire fingers, the robot pokes the hand to test it. Skywalker flinches, the wire pressing into his seemingly fleshy finger. Apparently, the hand works.
Standing up from the exam table to join Princess Leia, C3PO and R2-D2, Skywalker wiggles his new fingers, the prosthetic hand working and looking just like his own, the one he lost to a whooshing slice of Darth Vader’s neon-red light saber mere hours ago …
For the five or so people who haven’t seen “Star Wars,” that was a scene from the 1980 sequel, “The Empire Strikes Back.” It’s fiction, obviously. We don’t have light sabers to thwart foes, spacecraft that can maneuver through space at light speed or robots to tend to space wounds, as much of a blow this reality may be to the film’s ardent devotees.
But 28 years after the movie was made, are all of the futuristic abilities seen on screen still quite so unbelievably fictional? Actually, no. Researchers in the University of Florida colleges of Medicine and Engineering are getting closer to making at least one of the film’s sci-fi effects a reality – the ability to control an artificial limb as if it was your own.
“It’s becoming a reality,” says Justin C. Sanchez, Ph.D., an assistant professor of pediatric neurology in the College of Medicine and director of the Neuroprosthetics Research Group. “We’re designing electronics that we can interface with biological systems and we can use that to help people.
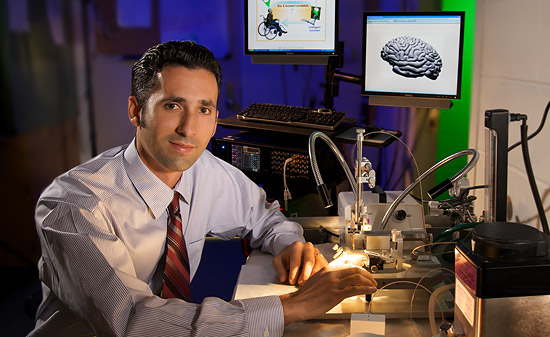
Dr. Sanchez and his team in the Neuroprosthetics Research group develop brain-machine interfaces. These devices are designed to enable paralyzed patients to control computers, prosthetic limbs and wheelchairs directly with their thoughts. In the laboratory, new bionic devices are designed to be implanted into the brain.
“There’s been kind of a revolution going on in the neurosciences and biomedical engineering. People are trying to take engineering approaches for directly interfacing with the brain. The hope is we can cure more immediately a variety of (conditions).”
The goal for Sanchez and his colleagues is to develop a super-small, implantable, wireless device that would allow a person to control a robotic limb with just their thoughts. Scientists across the globe are honing these technologies to try and perfect them for routine use in humans, including at UF, where researchers received a $2.6 million grant from the National Institutes of Health to design a tiny, low-power chip to test in rats in 2007.
“This is the most challenging project we’ve attempted,” says John Harris, Ph.D., a UF professor of engineering and the lead researcher on that project. “The ultimate goal is to develop a brain-machine interface that directly controls a robotic arm or a computer cursor. It’s very science fiction. (But) we’re taking small steps in that direction.”
But perhaps it’s Sanchez and his colleagues’ latest discovery that is the most “science fiction” of all. The team devised a way for a brain-machine interface to not only translate thought into motion, but also evolve with the brain as it learns.
Until now, brain-machine interfaces have been designed as one-way conversations between the brain and a computer, with the brain doing all the talking and the computer following commands. The system UF engineers created actually allows the computer to have a say in that conversation, too, according to findings published in June in the Institute of Electrical and Electronics Engineers journal IEEE Transactions on Biomedical Engineering.
“This idea opens up all kinds of possibilities for how we interact with devices,” Sanchez says. “It’s not just about giving instructions but about those devices assisting us in a common goal. You know the goal, the computer knows the goal and you work together to solve the task.”
So how does it work? Brain machine-interfaces are programmed with complex algorithms that interpret thoughts. But the algorithms, or code, used in current brain-machine interfaces don’t adapt to change, Sanchez said. So UF researchers developed an interface that used a system of rewards and goals. The rats they tested were trained to move a robotic arm toward a target with their thoughts. If they hit the target, they received a drop of water. The computer, on the other hand, received points. The closer a rat moved the arm to the target, the more points the computer received, giving it incentive to determine which brain signals led to the most rewards, making the process more efficient for the rat. Despite increasingly difficult tests, the rats got better and better as the brain-machine interface adapted to their thoughts, Sanchez says.

To determine a paralyzed patent’s intent to move from their thoughts, microelectrode arrays are implanted directly into the brain. “It’s not just about giving instructions but about those devices assisting us in a common goal,” said Justin C. Sanchez, PhD. “You know the goal, the computer knows the goal and you work together to solve the task.”
“We think this dialogue with a goal is how we can make these systems evolve over time,” Sanchez said. “We want these devices to grow with the user. (Also) we want users to be able to experience new scenarios and be able to control the device.”
Who knows if there will ever be space robots to attach our prosthetic limbs with wiry fingers, but the science of prosthetics has come a long way from the days when the choices were limited to peg leg or hook.
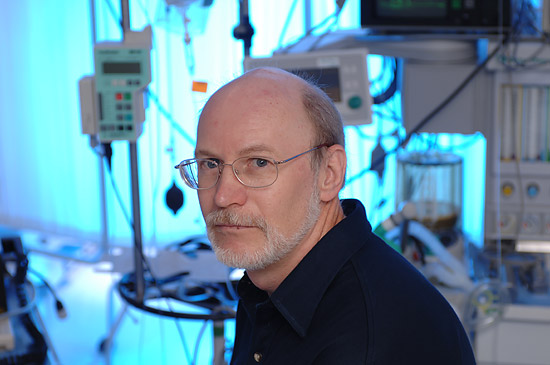
“Ultimately, we will get to the point where we’re bioengineering prosthetic limbs out of living material almost exclusively,” says William Ditto, Ph.D., chair of biomedical engineering in the College of Engineering. “Someday. And I think that day is not all that far in the future.”
Future Suture
Imagine. It’s the evening before you undergo risky, yet necessary surgery. You are preparing mentally and physically. Chances are your surgeon is doing the same, only he’s already poked around inside your body without making a cut.
How? Virtually.
It isn’t so far in the future where, through evolution, we acquire new powers. And just five or so years down the road — by using a few CT scans, simulated surgical tools, and a whole lot of math — your surgeon can practice each step of a surgical procedure through a virtual exact replica of your body.
Back to the (Near) Future
Surgical techniques can take years to perfect and also can prove challenging to teach and learn, so researchers at the University of Florida are working to improve training opportunities via simulation with one primary benefit in mind – patient safety.
The multidisciplinary team includes surgeons, biomedical engineers, mathematicians and experts in simulation and computer sciences.
“In surgery nothing is more dramatic than a knot that is set wrong or unable to hold the tissue correctly,” said Juan C. Cendan, MD, an associate professor of surgery at the College of Medicine, whose role is to translate the surgical experience into terms that can be mathematically reproduced for computer programming. “In some brands of surgery, like vascular surgery, the issue is immediate. GI surgery is perhaps not as immediate, but (the result) could be just as catastrophic if the knot is not set right.”
He added that minimizing the amount of time it takes to tie the knot is also crucial.
The surgical simulation research projects were initiated a few years ago under the leadership of former surgery chairman William G. Cance, MD, a professor of surgical oncology.
“Simulation of surgical procedures is absolutely critical to the future of surgery, as it provides new avenues of training while enhancing patient safety,” said Cance, who served as chairman of the department for more than five years. “As a department, we have taken a multifaceted approach to simulation, taking advantage of the expertise in our department as well as the UF expertise in computer engineering and mathematics.”
The team is working on three projects that will benefit the entire spectrum of surgical preparation, ranging from the medical student who aspires to one day be a surgeon to an experienced surgeon who could benefit from a simulated preparation for a complicated case. The projects are supported by funding from a National Institute of Biomedical Imaging and Bioengineering grant, a developmental seed grant from the university, a UF College of Medicine Chapman educational grant and the department of surgery.
Sergei Kurenov, MS, a computer simulation expert who leads the UF department of surgery’s surgical simulation group.
Sergei Kurenov, MS, a computer simulation expert who leads the UF department of surgery’s surgical simulation group, compares the importance of surgical training to pilots’ training needs.
“No pilot can fly without spending many hours flying on a simulator,” said Kurenov. “For me the vision is the same — a surgeon would not go into the operating room without first training with a computer simulator.”
Modifying a standard hand-held haptic device, designed to measure pressure applied by the user, Kurenov created attachment handles from real surgical tools.
Evaluating them on time and suture placement, one of the simulated programs will allow medical students to practice basic suturing technique until perfection is achieved. It is anticipated this program will be available to medical students in about a year.
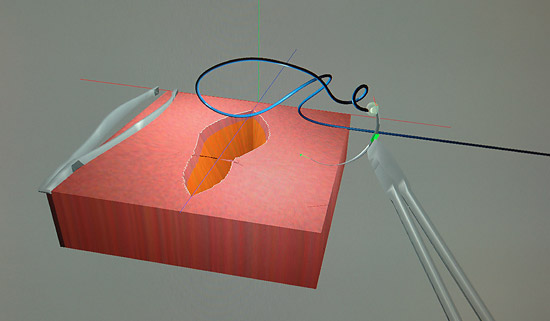
The visual on the monitor shows a skin wound; the coding behind the illustration is a mathematical grid that constructs a simulated model of what it would feel like to put a surgical needle through the various densities of elements such as skin, fat or muscle, as well as how these elements react to being sewn together.
Kurenov said each element in the grid represents a mathematical equation that corresponds to the density. He developed the math behind the grid, and Sergei Shabanov, PhD, an associate professor of mathematics, worked with the team to create the mathematical model for the simulation of the surgical thread.
“It’s a compilation of physical knowledge because we need to create the physical objects, and math and computer science,” said Kurenov, who once developed simulation programs for Russian MiG fighters. “Everything combined together creates the simulation.”

Kurenov explains the latest program to Juan C. Cendan, MD, an associate professor of surgery. Cendan’s role is to translate the surgical experience into terms that can be mathematically reproduced for computer programming.
For surgical residents, the team is focusing on the Endo Stitch device, used in minimally invasive surgeries. Kurenov adapted the device’s handle, which includes levers and buttons used to manipulate the laparoscopic needle, to be used with the simulation program.
Cendan said the Endo Stitch is a difficult instrument to learn and can prove challenging to teach, but the simulated program gives trainees a pretty good idea of the skills needed to use the tool. The team just made the advancement of incorporating tying knots into the training simulation.
“We are trying to create enough of a reality so that the surgical learner feels they are immersed in this experience,” said Cendan, who says the Endo Stitch simulator should be ready this year.
He added that it allows them to interact and see the relationship between anatomical structures, as well as the actual feel of them.
The team is currently working to expand the ‘feel’ element by having a program that would form CT scans into deformable, soft and flexible, anatomical organs.
This leads to TIPS, the final, collaborative project with Jorg Peters, PhD, a professor of computer and information science and engineering, and his SurfLab, which is working on the development of new algorithms for complex geometry. TIPS, or Toolkit for Illustration Procedures in Surgery, will create from CT scans virtual 3D illustrations of organs that reflect their varying densities.
“This is the holy grail of virtual surgical simulation,” said Cendan.
Peters’ idea for TIPS is to give a surgeon a flexible and convenient tool for the development of surgical illustrations of procedures. When complete, the toolkit will consist of libraries of virtual surgical instruments, anatomical organs and preprogrammed tools for easy to create tissue and 3D surgical scenes.
“We are creating a presentation tool, similar to a hypercharged word processor, that allows a top surgeon to explain key points of a complex procedure in a hands-on fashion,” said Peters. “We think force feedback in a 3D virtual environment will help practicing and future surgeons to learn new techniques.”
He added, the interdisciplinary effort between computational tool builders and practicing surgeons at UF promises to create unique educational tools.
Currently the SurfLab group is testing this concept on an adrenalectomy. The adrenal gland and kidney arteries are intertwined, contributing to a challenging procedure.
“It is very difficult to find the vessel so the surgeon should work very carefully with the instruments,” Cendan said. TIPS records each movement of the hand, so surgeons can evaluate the impact of their chosen steps.
TIPS also will provide a unique look at spatial relationships of organs, providing views from new angles as the virtual body is turned and tilted.
To get to their goal of being able to illustrate and offer the ‘feel’ of any procedure it is going to take another step that the collaborative team still needs to figure out.
Staying true to the real meaning of educator, the team is focusing on making the program affordable so that it is available to every surgeon, not just the elite.
“There are other simulation programs out there that are very expensive and the applicability is very limited,” Cendan said. “This will have an open format so you can put the structures together however you want for whatever you are trying to illustrate.”
So back to that night before surgery – sleep easy – because with each passing day progress is being made with your safety at the forefront.
–
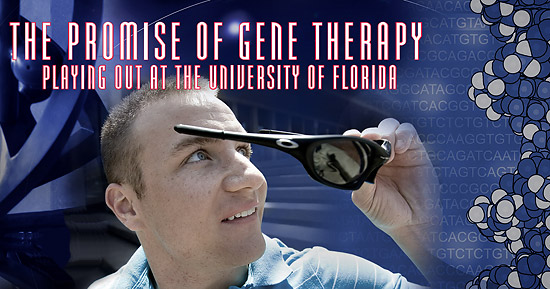
Three decades have passed since gene therapy pioneer William W. Hauswirth, PhD, and colleagues at UF began work on a virus that could safely deliver corrective genes into living animals. By the mid 1980s scientists began to publicly extol the promise of gene therapy.
But the field encountered its share of obstacles. For one, the much-heralded therapies did not arrive quickly enough to meet high public expectations. The principles of gene therapy were sound, but secondary issues such as how to handle immune responses to the therapy were daunting. In addition, a small number of adverse health events during trials further slowed the process.
Some scientists became discouraged. Others assiduously continued their work – including Hauswirth.

William W. Hauswirth, PhD, the Rybaczki-Bullard professor of ophthalmic molecular genetics at the College of Medicine
His years of research and persistence paid off this year when the gene-transfer technique he and his collaborators developed not only proved safe in humans, it restored some vision in patients with a rare, incurable form of blindness.
The patients-one woman and two men ranging from 21 to 24 years old with a type of hereditary blindness called Leber congenital amaurosis type 2 – volunteered to test the safety of the gene therapy in a phase 1 clinical research study conducted by UF and the University of Pennsylvania with support from the National Eye Institute.
The subjects in the study said the vision in their treated eyes was slightly improved in dim lighting conditions, as reported in a paper published in Human Gene Therapy in September.
“The lighted dial on my bedside dial is now too bright,” remarked one patient after her treatment.
“I saw fireworks for the first time this 4th of July,” said another.
“The patients report seeing brighter areas and perhaps some images, but basically the message is that this treatment is fully safe,” said Hauswirth, the Rybaczki-Bullard professor of ophthalmic molecular genetics at the College of Medicine.

Barry Byrne, MD, PhD, director of the Powell Gene Therapy Center, develops new genetic therapies for cardiovascular disease and says the future will include very specific treatments aimed at genetic causes of disease.
Instrumental in the apparent success of this gene-therapy trial and others being conducted at UF are College of Medicine geneticists Nicholas Muzyczka, PhD, and Kenneth Berns, MD, PhD, director of the UF Genetics Institute. In 1992 Muzyczka and Berns patented a form of the gene-carrying adeno-associated virus that is capable of introducing foreign DNA into mammalian cells.
“UF is one of the world leaders in gene therapy,” says Dr. Barry J. Byrne, a professor of molecular genetics and the director of UF’s Powell Gene Therapy Center. “Treatments designed to correct these fundamental errors are what gene therapy is all about. In the future, we hope that very specific treatments for disease are aimed at the genetic cause of the disease.”
Mark Brantly, MD79, director of the College of Medicine’s Alpha-1 Research Program, began phase 1 clinical trials in 2004 for people suffering from alpha-1 antitrypsin deficiency, an inherited disorder that can cause lung disease in adults and liver disease in children and adults. Alpha-1 antitrypsin is a protein that protects the lung. Because of a gene problem, some people have little or none of the protein.
Brian Keebaugh, of Kathleen, Ga., receives experimental gene therapy at UF from Brantly in an effort to restore the alpha-1 protein in his body. And it is Brantley who is impressed with Keebaugh and others like him who participate in the trials.

Mark Brantly, MD79, the director of the College of Medicine’s Alpha-1 Research Program injects good, healthy genes in patient, Brian Keebaugh, during a UF clinical trial to replace the absence of protein.
“They are quite remarkable,” he said. “Gene therapy patients are focused on developing therapies for future patients.
“They are very courageous and very brave at what they do.”
Dale Turner is one of the courageous patients. The law student from Oshawa, Ontario, became the first Canadian to undergo the gene-therapy procedure to treat his blindness.
Three days later he shed tears of joy as he caught his first glance of the bright blue sky. It was an emotional moment, described the 21-year-old, who had approximately 10 percent of his vision before the experimental therapy.
“I forgot how blue the sky can be,” he said.